At Home
Whitening:
Current status
and recommendations for dentist prescribed, at home tooth whitening.
Since its introduction in1989, night guard vital bleaching
(often called dentist-prescribed, at home whitening using a10% carbamide per-oxide in
custom-fitted tray has made a significant impact on the practice of esthetic and
restorative dentistry. Over time, a significant amount of laboratory and clinical
research, as well as numerous case reports have supported the technique. The American
Dental Association (ADA) established its guidelines for safety and efficacy in 1994.Many
of the more recent articles provided a better understanding of the whitening process and
its applications. A1999 ADA statement included the following .the preponderance of
scientific evidence currently available in the literature supports the safety of the home
-use and dentist- prescribed tooth- bleaching products when properly applied and
monitored.
Material used: 10%carbamide peroxide. Almost
all the major research in the world has been conducted on 10%carbamide peroxide, and only
10% carbamide products (3% hydrogen peroxide) currently have the approval for at-home use.
Recently, the Food and Drug Administration (FDA) approved the use of 3% hydrogen peroxide
in toothpaste for the life of the patient as safe, which adds confidence to using the
dentist-prescribed, at-home whitening technique. At this time, there is no significant
research to support the at-home use of concentrations of carbamide peroxide higher than
10%, or hydrogen peroxide higher than 3%. This does not mean that other products are not
safe, but it does mean that it is not known what degree of safety and efficacy exists.
Duration and Extent of Treatment: Most
products available promise quick and easy results in 14days or less. This may be true for
some patients, but success depends more on the patient than product. The original night
vital bleaching article recommended 2 to 6 weeks of treatment with10% carbamide peroxide.
It is important for the dentist to prepare the patient for treatment that will last longer
than a few days, in case the patients teeth are not as responsive as anticipated,then the
patient will be more likely to comply with home treatment until the best colour change is
achieved rather than become discouraged. If the colour change occurs in a few days, the
patient is even happier.
Application: Nightly treatment is the most
effective use of material per application, and patients in extended treatment comply
better with night wear. Clinical studies have shown the 10%peroxide material to still be
active in the tray at 4 hours and even after 10 hours of application. Daywear can achieve
the same results but may take longer or use more material. Its has been shown in the
laboratory that higher concentrations of material may result in faster lightening.
However, clinically, the higher concentrations invite more sensitivity, which has been
cited as the only real detriment to compliance by the patient.
The most effective whitening recommendation is the use of
10%carbamide peroxide applied nightly until the teeth either reach the desired shade or
cease to change shades over a week’s treatment. For tetracycline stained teeth, the
patient should be willing to commit to at least 2 months of treatment, continuing up to 12
months if needed.
Short –Term treatment: Treatment time
can be very short for some patients, but the dentist cannot predict either the length of
treatment or the final shade out come. Sometimes it has been observed that the teeth
whiten in as little as 3 nights .The dentist can help patients choose a method that best
fits their lifestyle, goals for treatment(including time and cost), parafunctional habits
(bruxism and gagging),etc.
Long-Term treatment: In some cases,
whitening can be a long -tem treatment. Extended treatment times of 2 to 6 months or
longer have been reported. These extended treatment times can be necessary for stubborn
stains, such as nicotine or tetracycline. Discoloration in the gingival third of the tooth
is less responsive to whitening, especially in the case of grey tetracycline staining, in
these situations, patients must be prepared to view treatment as a longer- term
commitment, much like a weight- loss or exercise program.
Fees: The national average fee for one-arch
/ dual arch whitening depends on geographic location, office overhead, range and length of
treatment , and type of whitening material used. The fees for extended treatment can be
based on the amount of material used per month (which depends on the arch size, the tray
design, and the patients application technique) and the number of months treated. The
patient can be seen monthly to evaluate progress, with a fee for each monthly recall to
include the amount of material necessary for another months treatment. In this manner, the
patient pays for the treatment as it progresses, without the dentist having to change
either an unreasonably high or low fee at the outset of treatment.
Sensitivity: Probably the only major
detriment to whitening is the occasional occurrence of sensitivity during treatment.
Examining all the available data from double-blinded clinical trials indicates that in the
treatment groups, about 55%to 75% of the patients experience sensitivity. This sensitivity
may be a result of the easy passage of the hydrogen peroxide and urea through the enamel
to the dentin, which can occur in a matter of minutes. This easy passage also explains why
we are able to change the internal colour of the tooth, and possibly how sensitivity is
related to the pulpal response to peroxide. The issue of sensitivity is one of the many
reasons why patients should be under professional supervision.
Many advertisements claim superiority in sensitivity
reduction with a particular whitening product, but to date there are no published
scientific studies supporting these claims. In fact, if one evaluated the best
evidence-based studies on whitening, all studies report sensitivity as a side effect. This
sensitivity does not necessarily interrupt the treatment, and may last only 1 day.
Also, most studies indicate that in the placebo group (those
not exposed to the carbamide peroxide ), generally 30% to 35% experience sensitivity,
perhaps as a result of tray rigidity, or the flavour, base vehicle, or other ingredients
in the placebo.
Even more significant is that one study reported that wearing
the tray alone (with no treatment or placebo product applied) resulted in 15% to 20% of
the patients develop sensitivity. The forces of the tray, the forces of occlusion, the
insertion path of the tray, and pressure from saliva can elicit a sensitivity response.
Data from these studies seem to indicate that sensitivity is
a multi factorial event related to both the patient’s host response as well as the
material, the tray, the arch anatomy, and treatment time. No one product has demonstrated
superiority in sensitivity reduction of any significance. In fact, it may be an advantage
to the practice to have more than one product available. The two products could be the
same concentration of carbamide peroxide, but be very different in base composition,
vehicle, flavouring, etc. If a patient has problems with a particular material, the other
material could be substituted.
One retrospective study indicated that the only predictors
for sensitivity were either the application of the product more than once per day, or a
history of or examination revealing sensitive teeth. The age or sex of the patient, the
presence of cracks, exposed dentin, caries, pulp size etc. do not help the dentist predict
who will have sensitivity. The best option is to inform patients that they have a good
chance of experiencing sensitivity, and that it is usually mild, short lived, and ceases
on termination of the treatment.
Passive and Active Treatment for sensitivity: There
are two methods to consider for the treatment of sensitivity related to whitening :
Passive and active. The passive method consists of altering the treatment time, frequency,
or duration to find a comfortable solution for the patient.
The active method employs either the use of fluoride or
potassium nitrate applied in the tray as a pre-treatment or at the onset of sensitivity.
It is important to distinguish between the action of these two materials.
Flouride: Fluoride is basically a tubular.
It occludes the dentinal tubules, restricting the ingress of fluid flow as described in
the hydrodynamic theory of pain. A neutral fluoride has been the recommended treatment
either applied in the whitening tray, in the office, or through brushing with a
prescription fluoride toothpaste.
Potassium Nitrate: Potassium nitrate acts on
the tooth in a different manner to reduce sensitivity. It passes freely through the tooth
to the pulp and either prevents the repolarization of the nerve after firing, or aids in
the release of nitric oxide. Either way, the effect is directly on the nerve, resulting in
a calming effect on the tooth. This effect has been long known and most of the
desensitising toothpaste contain potassium nitrate. Generally, brushing with a potassium
nitrate - containing toothpaste takes about 2 weeks to reduce sensitivity. Five percent
potassium nitrate is the maximum concentration approved by the FDA. In patients
experiencing sensitivity during whitening, potassium nitrate can be applied in a tray for
10 to 30 minutes before or after whitening, or when the sensitivity occurs.
Other Treatment Options: The only side
effect so far associated with using desensitising toothpaste in a tray is tissue burn in
some patients. Another option available to the dentist is to supply a fluoride gel
manufactured specifically for tray application. These materials can be applied as needed,
or alternated with the whitening treatment.
Contraindications for At-Home Whitening:
- Unrealistic Expectations.
- Unwilling to comply with the treatment.
- Not willing to tolerate the taste of the product.
- Excessive restorations not needing replacements.
Gaurded Prognosis for Whetening:
- History of presence of sensitive teeth
- Extremely dark gingival third of tooth that is visible during
smiling.
- Extensive white spots.
- Bruxism.
- Exposed root surfaces.
- Attritioned teeth.
Tray Fabrication: A good alginate impression
is the start of a good whitening tray. Before seating the impression, lightly wipe
alginate on the facial of the central incisors and the occlusal surfaces of the posterior
teeth to eliminate voids in the impression. All of the teeth and 2 mm to 3 mm of gingivae
should be captured in the impression. The palate is not needed.

|
Showing a lower tray to be used for upper
impressions. |
| Impression of both the arches, excess algenate
is cut with BP knife before pouring the impression |

|

|
Radically trimming the cast provides good tray
fabrication. The ideal cast is trimmed so that the central incisors are perpendicular to
the base and there is no vestibule or palatal coverage. |
| Resorvoirs are made on the labial and buccal
surfaces of teeth to be bleached leaving 1mm short at the cervicle margins , these
reservoirs extend to the palatal side of ant teeth . Though some manufacturers also say
that the reservoirs are not needed to be effective. |

|

|
Ultravac machine for tray fabrication , this
heats the tray and then adapts it by suction. |
| The vacuum-forming machine is used to adapt the
soft tray material onto the dry cast. Proper tray materials are thin, soft, and when
heated, do not smell, smoke, or buble. The newly formed tray should bench cool or be
placed under cool running water before trimming. |

|

|
There are three tray designs that can be cut :
1) nonscalloped on the facial and lingual. 2) scalloped on the facial and lingual. 3)
nonscalloped on the lingual, scalloped on the facial. The tray cut non scalloped on facial
and lingual / palatalas shown with sharp scissor. |
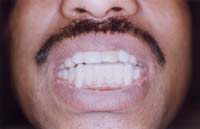
| Upon insertion of the nonscalloped tray, ensure
that no tissue blanching occurs. Tray edges should be smooth, and the insertion path
should not enter into undercut areas. Relief for frenum movement should be provided. |
|
Possible Causes of Extrinsic
Discolouration:
- Bacteria Green, Orange, Black, Brown.
- Beverages & Coffee Brown, Black.
- Tea Brown, Yellow
- Tobacoo Brown, Black
- Chlorhexidine Brown, Yellow
Possible Causes of Intrinsic Discolouration:
- Aging Yellow, Gray
- Internal resorption Pink
- Trauma Gray, Black, Yellow, Brown, White spots
- Tetracycline Gray, Yellow, Brown, Blue
- Non Vital tooth Gray, Brown, Black.
- Caries Gray, Black